
Breakthrough in Cancer Prediction with Nano Informatics and AI: A recent study has introduced a novel method combining nano informatics and machine learning to precisely predict cancer cell behaviours, enabling the identification of cell subpopulations with distinct characteristics like drug sensitivity and metastatic potential. This research could transform cancer diagnosis and treatment, enhancing personalised medicine by facilitating rapid and accurate testing of cancer cell behaviours from patient biopsies and potentially leading to the development of new clinical tests to monitor disease progression and treatment effectiveness.
In an important advance in the fight against cancer, a research team from The Hebrew University has developed a new method to predict the behaviour of cancer cells with high accuracy. This innovative approach, combining nano informatics and machine learning, could revolutionise the diagnosis and treatment of cancer by allowing for the rapid identification of cancer cell subpopulations with varying biological behaviours.
In a novel study led by doctoral student Yoel Goldstein and Prof. Ofra Benny from the School of Pharmacy in the Faculty of Medicine, in collaboration with Prof. Tommy Kaplan, Head of the Department of Computational Biology at the School of Engineering and Computer Science at Hebrew University, The Hebrew University, an innovative method was developed to predict cancer cell behaviour using nano informatics and machine learning. This discovery may lead to a significant breakthrough in cancer diagnosis and treatment, enabling the identification of cancer cell subpopulations with different characteristics through simple and quick tests.
The initial phase of the study involved exposing cancer cells to particles of various sizes, each identified by a unique color. Subsequently, the precise amount of particles consumed by each cell was quantified. Machine learning algorithms then analysed these uptake patterns to predict critical cell behaviours, such as drug sensitivity and metastatic potential.
“Our method is novel in its ability to distinguish between cancer cells that appear identical but behave differently at a biological level,” Yoel Goldstein elaborated and explained “This precision is achieved through algorithmic analysis of how micro and nanoparticles are absorbed by cells. Being capable to collect and analyse new types of data brings up new possibilities for the field, with the potential to revolutionise clinical treatment and diagnosis through the development of new tools.”
The research has paved the way for new types of clinical tests that could significantly impact patient care. “This discovery allows us to potentially use cells from patient biopsies to quickly predict disease progression or chemotherapy resistance,” stated Prof. Benny. “It could also lead to the development of innovative blood tests that assess the efficacy of targeted immunotherapy treatments as example.”
Current tools for predicting and detecting cancer often lack accuracy and efficiency. Traditional methods like imaging scans and tissue biopsies can be invasive, costly, and time-consuming, leading to delays in treatment and potential misdiagnoses. These approaches may not capture the dynamic nature of cancer progression and can result in limited insights into the disease’s behaviour at a cellular level. Consequently, patients may experience delays in diagnosis, suboptimal treatment outcomes, and increased psychological distress. This highlights the urgent need for more effective and non-invasive diagnostic tools, like the recent breakthrough achieved by researchers at The Hebrew University, which represent a significant advancement in personalised medicine, providing hope for more effective and customised treatment strategies for cancer patients.
The research paper titled “Particle uptake in cancer cells can predict malignancy and drug resistance using machine learning” is now available in Science Advances and can be accessed here
Researchers:
Yoel Goldstein1, Ora T. Cohen1, Ori Wald2, Danny Bavli3, Tommy Kaplan4,5, Ofra Benny1
Institutions:
1) Institute for Drug Research, The School of Pharmacy, Faculty of Medicine, The Hebrew University of Jerusalem
2) Department of Cardiothoracic Surgery, Hadassah Medical Center, Faculty of Medicine, The Hebrew University of Jerusalem
3) Department of Stem Cell and Regenerative Biology, Harvard Stem Cell Institute, Harvard University
4) School of Computer Science and Engineering, The Hebrew University of Jerusalem
5) Department of Developmental Biology and Cancer Research, Faculty of Medicine, The Hebrew University of Jerusalem
Picture
Illustration
Credit: Made by Ofra Benny by OpenAI software DALL-E

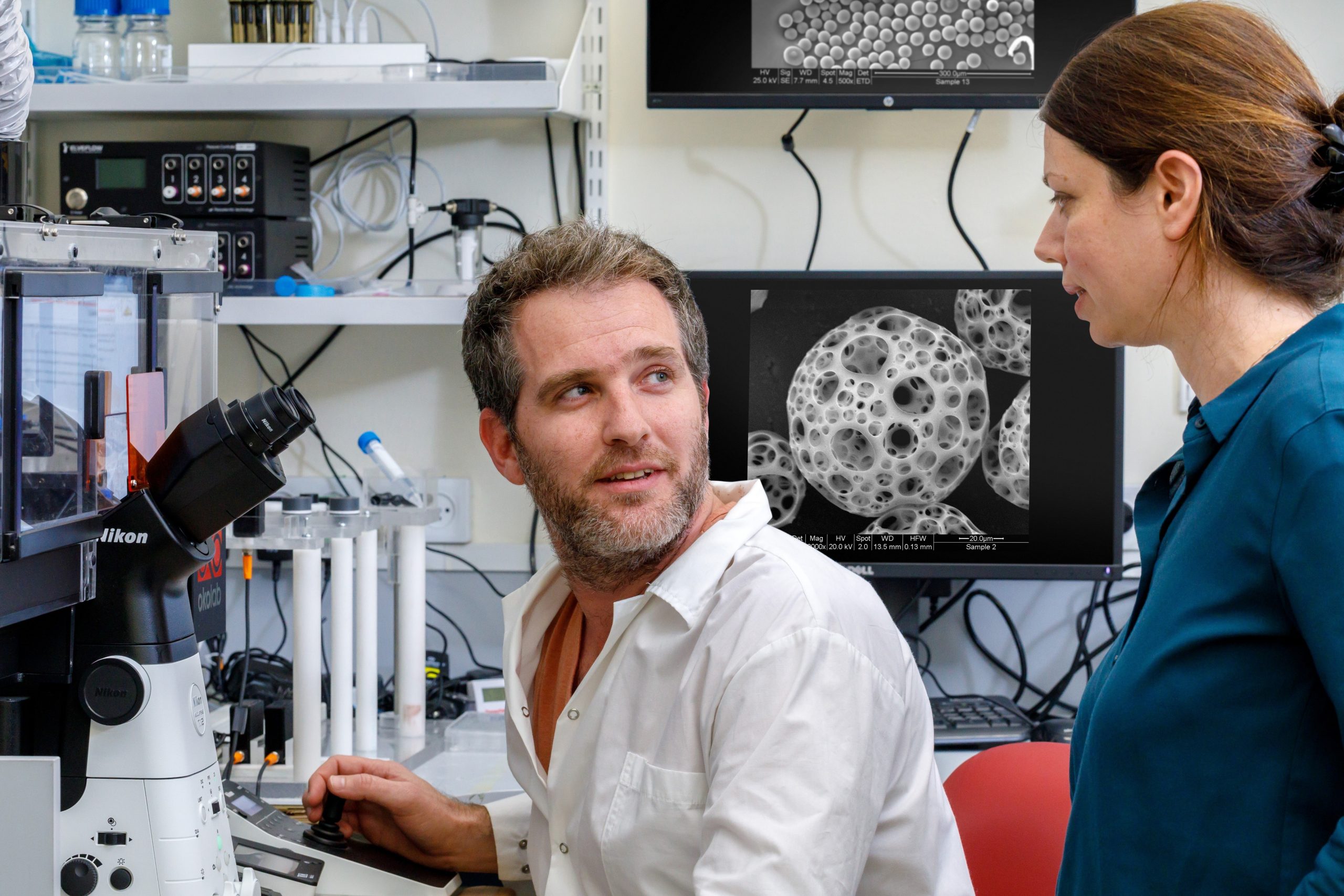
Title: Yoel Goldstein and Ofra Benny in the Lab
Credit: Yoram Aschheim
Disclaimer: In these challenging times of war and crisis, Hebrew University of Jerusalem is resolute in its dedication to advancing research and education. We stand in full support of the brave individuals on the frontlines, safeguarding our nation and the well-being of all Israelis, and extend our deepest gratitude and unwavering solidarity to our community and fellow citizens. Together, we shall prevail against the challenges that confront us, and our shared commitment to the well-being of all Israelis and the pursuit of knowledge remains resolute.
The Hebrew University of Jerusalem is Israel’s premier academic and research institution. Serving over 23,000 students from 80 countries, the University produces nearly 40% of Israel’s civilian scientific research and has received over 11,000 patents. Faculty and alumni of the Hebrew University have won eight Nobel Prizes and a Fields Medal. For more information about the Hebrew University, please visit http://new.huji.ac.il/en.
